NCNC Annual Meeting
NCNC held its Annual Meeting September 8, 2023 at the Cecil G Sheps Center for Health Services Research, University of North Carolina at Chapel Hill.
We welcomed two new partners at the annual meeting: The Practice-Based Equity Research Network located at North Carolina Central University, and the Piedmont Health Services Research Team.
Matt Simpson, MD, MPH who has worked in practice-based research in Colorado and now works at the Agency for Healthcare Research and Quality , Division of Practice Improvement in the Center for Evidence and Practice Improvement, gave a talk about their interest in supporting practice-based research and potential opportunities for funding.
Skip Cummings is 2023 Jim Bernstein Community Health Career Achievement Awardee
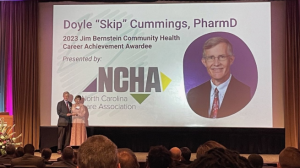 The Foundation for Health Leadership & Innovation presented Skip Cummings, PharmD with the 2023 Jim Bernstein Community Health Career Achievement Award.
The Foundation for Health Leadership & Innovation presented Skip Cummings, PharmD with the 2023 Jim Bernstein Community Health Career Achievement Award.
Skip is a professor of Public Health and Family Medicine at East Carolina University. Skip was recognized for his decades of work to improve health in North Carolina’s rural communities. Skip is the Berbecker Distinguished Professor of Rural Medicine at ECU, where he has taught for 35 years.
Survey for Primary Care Providers about improving care for patients with Rare Cancers.
Rare cancers account for 27% of all cancers and 25% of all cancer deaths. Primary Care Providers in rural and underserved communities are often the first health care professionals that patients see when they have symptoms of rare cancers.
Primary Care Provide rs (particularly those serving patients in rural settings) are invited to take a 15-minute survey to share their knowledge and experiences on the diagnosis, referral patterns and care coordination for patients with IBC and other rare cancers as well as the impact of COVID-19 and telehealth on caring for patients. This information will help us develop resources to help support providers care for their patients. For a limited time, those who complete the survey will receive an Amazon gift card
rs (particularly those serving patients in rural settings) are invited to take a 15-minute survey to share their knowledge and experiences on the diagnosis, referral patterns and care coordination for patients with IBC and other rare cancers as well as the impact of COVID-19 and telehealth on caring for patients. This information will help us develop resources to help support providers care for their patients. For a limited time, those who complete the survey will receive an Amazon gift card
https://redcap.duke.edu/redcap/surveys/?s=YYKM7XELT9EXAK3J
MAHEC Research Certificate
This training is co-sponsored by the Mountain Area Health Education Center and the UNC-Chapel Hill Department of Family Medicine. It is funded in part by the John T. Henley Sr. Endowment Fund.
The MAHEC Research Curriculum consists of 8 separate independent-learning Modules. If you complete all 8 Modules, you may self-attest to receive a Certificate of Completion.
The 8 modules are:
- Define a Research Question using the PICOT framework (Population, Intervention, Comparison, Outcome Timeframe)
- Searching the Literature
- Critical Appraisal of the Literature
- Quantitative Research
- Qualitative Research
- Protection of Human Subjects
- Data Management
- Structuring a Research Paper
Each module is designed to take 30-45 minutes to complete. Bonus Activities will add an additional 20 minutes. Completing the full curriculum should take between 4.5-7 hours. https://ncahec.libguides.com/MAHEC/ResearchCurriculum
Practice Facilitation Paper
 Kent Sutton, MPH, a fourth year medical student at Duke University was the lead author of a manuscript “Implementing Practice Facilitation in Research: How Facilitators Spend Their Time Guiding Practices to Improve Blood Pressure Control” published in Implementation Science Communications. https://implementationsciencecomms.biomedcentral.com/articles/10.1186/s43058-023-00470-y
Kent Sutton, MPH, a fourth year medical student at Duke University was the lead author of a manuscript “Implementing Practice Facilitation in Research: How Facilitators Spend Their Time Guiding Practices to Improve Blood Pressure Control” published in Implementation Science Communications. https://implementationsciencecomms.biomedcentral.com/articles/10.1186/s43058-023-00470-y
Kent collaborated with the team at Cecil G Sheps Center for Health Services Research on the Southeastern Collaboration to Improve Blood Pressure Control research study. The paper focuses on using Practice Facilitation (PF) as a study intervention.
Kent says, “This project is meaningful to me because our work underscores that PF is an innovative intervention in health care delivery that can address real-world challenges faced by practices in the community. We hope readers will be inspired to learn more about PF and use these results to design and test PF and other quality improvement interventions that can transform how we deliver health care services to patients in need.”
Our publication in Implementation Science Communications focused on the practice facilitation (PF) intervention in the trial. We investigated the time the study’s practice facilitators (PFs) allocated to various activities and responsibilities as they guided study practices in implementing PDSA activities including the time PFs spent driving to practice sites, working on-site with staff and clinicians, and communicating remotely with practice staff. We found that PFs spent significant time traveling to rural practices and primarily worked directly with practice staff on-site. PFs were able to successfully execute their duties without requiring significant time. PFs also greatly relied on remote communications.
Our results are noteworthy because they highlight that PF is a dynamic intervention that can be tailored to practices’ individualized needs. These findings may be useful to researchers and business leaders who design, test, and implement efficient facilitation services. Similarly, our results provide key insights into how to optimize in-person vs. virtual practice facilitation services in the post-pandemic era.
Re-Think the Strip Cost Paper
Lisa Spees, PhD, published A Cost Analysis of Rethink the Strip De-implementing a Low-value Practice in Primary Care in the journal Medical Care
The study detailed the costs for different implementation strategies used to de-implement the low value practice of daily glucose testing in patients with well-controlled type 2 diabetes.
https://journals.lww.com/lww-medicalcare/pages/default.aspx
Acknowledgements
NCNC would like to thank UNC’s Cecil G. Sheps Center for Health Services Research and the NC Translational and Clinical Sciences Institute for all they do that make our work possible.